Help! I have Essure and I never knew it could cause issues, what can I do?
Are you suffering any of the listed side effects? They’re all on the Side Effects page. Check out the Resources page for a downloadable list that you can print and take to your GP.
If you are, then your GP is the first port of call. Stay calm and factual, and explain to them what Essure is, how it works (lots of doctors have no idea!) and why you believe it’s causing you problems.
Keep a symptom diary; record how you feel, what happens, and when.
Fully expect your doctor to consider that it might not be Essure that is making you ill. A decent doctor is going to check out every possible cause, and eliminate them all, before they consider Essure.
Hopefully this may mean that after tests and basic examinations, you are referred for either a scan to see if anything obvious is going on internally, or directly to a gynaecologist.
Take your list of side effects and your diary. You will also find a letter to your gynaecologist on the Resources page that you can download and print.
Again, expect a decent doctor to rule out any other possible cause. They wouldn’t be doing their jobs right if they didn’t do this. However if anyone at hospital is outright rude, dismissive, won’t keep you informed, or makes you do something you don’t want to, then SPEAK UP. Use your hospital’s PALS advocacy service and seek help from the Essure support groups on Facebook, or email us here.
Imaging
Before removal is agree, push to get some imaging done. An ultrasound scan is great but even a trans-vaginal ultrasound won’t show the location of your Essure implants clearly enough for a gynaecologist to decide how best to remove them.
Ideally you need a pelvic x ray or at best, a CT scan – see the below graphic.
.
Once your gynae can see what’s going on they can decide on the “grade” of positioning you have. This determines how much of the surrounding pelvic organs have to be removed. Grades run from 1 to 4, with Grade 2 being “correct” positioning. If you have been told that your Essures are in the correct place, then you are Grade 2. This means that part of the Essure implant is trailing into your womb. Therefore you are NOT a suitable candidate for a salpingectomy (removal of the fallopian tubes only). If your gynaecologist suggests this, then be wary – they may be planning on pulling the coils out which is a bad idea.
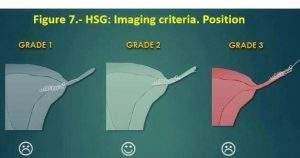
Grade 4 is not shown here, but infers complete migration into the abdominal cavity.
Removing Essure
Essure isn’t meant to be taken out. It’s permanent. This means that getting rid of it is a tricky procedure and there are ways that it should NOT be done.
If your surgeon says that they can remove it by pulling it out, they are wrong.
This can cause Essure coils to stretch, break and fracture. It is possible to leave bits of metal and PET fibres behind. You don’t want this to happen. If your surgeon suggests this, contact us.
Removing Essure is normally done by something called a salpingectomy – this means removing the fallopian tubes. Depending on where the Essure coils are in the tubes, some or all of the uterus may need to be removed at the same time. This is a hysterectomy.
Hysterectomies can be done in several ways. Generally speaking, a laparoscopic (keyhole) hysterectomy is not recommended for Essure patients, because in order to remove the uterus it must be morcellated (cut into pieces to get it out of the small openings created for keyhole surgery). Morcellation can chew up the coils and again, spread fragments. Discuss this with your consultant.
*disclaimer* We’re not doctors. Run all of this past your consultant and take on board what they have to say – but if they know nothing about Essure at all, point them to this site (especially the Resources page).